Hi there!
I am calling this version of my IVF Journey the “Cliff Notes Addition”.
Basically, when our infertility issues began, I started documenting the journey in a private unpublished blog. After about 10 months of documenting I hit over 13,000 words and the journey still wasn’t over..
I began worrying no one would ever read, or enjoy, the long saga that was our story. But because I put so much blood, sweat, and tears into the process, and I documented every bit of it, I wasn’t willing to completely ditch that version and start over with an easier to read one.
I shared these concerns with my step-mama who suggested I maybe write a short and sweet “cliff notes” version and if anyone wanted to read through the details, I could provide a link to that version of the story, which you can find HERE.
Even though I worked so hard on the original, I honestly prefer this version more. So I hope you agree!
Honestly, the long version is probably geared more for someone who is also going through infertility, and exploring IVF, or you are about to start IVF and you’re curious what the process will be like.
Even after deciding to make this cliff notes version, it still ended up longer than I anticipated even though I tried my hardest to keep it short sweet and to the point.
sorrrrrry
So a couple of things before I get started.
- I will occasionally copy and paste from my long version. So if you read both, just know you will probably see some of the same content.
- Just like in my original version, here is my official WARNING that this post will contain adult words and topics, such as, but not limited to; vagina, penis, semen, sex, the occasional profanity, and basic anatomy talk.
If you cannot handle these topics/words, or you are under the age of 18, this IS NOT the reading material for you. - If you are unaware about what the heck IVF is, or you have at least figured out it has something to do with making a baby but the logistics of it are still unknown, here is the link for you – IVF 101.
You can also spend 12 hours reading my painfully detailed version where I literally chronologically explain each and every step, process, procedure, medication, and emotional meltdown.
Enjoy!
Lets just jump right on in
You could say our relationship with infertility technically began when Mike and I fell in love and began talking about a future together.
Mike came into our relationship with a former vasectomy and I brought with me a desperate desire for one more child. We were both very open and honest about these two conflicting circumstances and ultimately Mike was comfortable with bringing one more (he used to joke about two more) children into the world.
Some would find this perplexing as we already have a pretty big blended family, with many dynamics, and age gaps not only between me and my husband, but between siblings as well.
But it was okay with us, and ultimately it’s our choice and journey, so if we weren’t bothered you have no business being bothered either.
Moving on..
After waiting just shy of a year for Mike to be able to get his vasectomy reversal (gotta love waiting on military medicine) we finally had the procedure in February of 2019. After surgery we needed to wait four weeks and then we were free to start trying for Baby Dodd.
In my detailed version of this story I dive into how difficult and minimally successful vasectomy reversals are. There are a lot of factors against you when attempting to reconnect those “pipes” and honestly we were blissfully ignorant of how low our chances of success were going to be.
Knowing what we know now, I think we would have attempted IVF from the very beginning and not wasted time with the reversal..
But we did the surgery and scheduled his first semen analysis for 3 months later, which was the end of May.
For 3 months leading up to the first analysis we aggressively and relentlessly tried every month.
This wasn’t a situation of “ohhh if it happens it happens“. From the first month of trying I was using ovulation test trips and attempting to perfectly time sex during my hormonal peak.
When that didn’t work I purchased a Basel Body Thermometer (BBT for short) and used that along with my ovulation test strips and timing sex around these windows.
We even purchased a microscope in hopes of seeing sperm on our own and not waiting for that first analysis and I was reading crazy at home methods to increase our chances; like eating high fertility foods, taking supplements, the whole 9 yards.
And then we got the formal semen analysis results back.. all of his stats were at 1%.
Not good..
Granted, we just received a copy of the results, none of this or our options were discussed with Mike’s urologist.
To be honest, it took two months to even be seen with the urologist to discuss what the results meant. So June and July were a very intense and an upsetting time in our household.
I knew Mike had no control over how his body was healing post surgery. But I was seriously angry and frustrated. Not necessarily with Mike, but the situation as a whole, it just felt so incredibly unfair.
I had waited and responsibly not added any more children to my life, no matter how desperately I wanted them or wanted Ryleigh to grow up with a sibling, until I was in a stable healthy marriage with financial security. Now that I was finally there and I was actually ready, poof! It felt like everything I waited so long for was gone.
So at that August appointment with his urologist, it was explained that sperm was in fact present but they only had 1% motility. Meaning, those little dudes just weren’t going anywhere.
It’s even safe to assume that there may be scar tissue at the re-connection that is damaging the sperm tails as they pass through and/or creating a partial blockage.
His doctor basically said there is enough sperm present to technically get me pregnant, but the chances of it happening on its own with us just trying at home were very very low odds. So he wrote us a referral to be seen in San Diego at the Military Infertility Clinic.
We had our first infertility appointment September 4th in San Diego. It is important for you to know that we live in Orange County, specifically San Clemente, CA. So for us to get to San Diego WITH TRAFFIC (god forbid there is an accident that locks up the highway) it can easily be 1 hour 20+ min drive ONE WAY. This detail is going to be important soon..
The initial appointment went well, the doctor confirmed that with Mike’s current sperm situation, we would be looking at IVF.
I guess we could have tried the less invasive and definitely cheaper option of IUI. But since his swimmers weren’t really swimming, and with IUI they are still expected to do a little bit of work, it probably would have been a huge waste of time.
Real quick – there are two primary approaches to getting pregnant when struggling with infertility.
- Intrauterine Insemination (IUI) is a fertility treatment that involves placing sperm inside a woman’s uterus to facilitate fertilization. The goal of IUI is to increase the number of sperm that reach the fallopian tubes and subsequently increase the chance of fertilization.
This is often referred to as the “turkey baster method”.- In vitro fertilization (IVF) is a complex series of procedures used to help with fertility or prevent genetic problems and assist with the conception of a child.
During IVF, mature eggs are collected (retrieved) from ovaries and fertilized by sperm in a lab. Then the fertilized egg (embryo) or eggs (embryos) are transferred to a uterus. One full cycle of IVF takes about three weeks. Sometimes these steps are split into different parts and the process can take longer.
IVF is the most effective form of assisted reproductive technology. The procedure can be done using your own eggs and your partner’s sperm. Or IVF may involve eggs, sperm or embryos from a known or anonymous donor. In some cases, a gestational carrier — a woman who has an embryo implanted in her uterus — might be used.
Okay, now you are caught up on reproductive technology, or so I hope.
Next we had to discuss costs of IVF treatment. On average IVF costs around $20,000+. But because we were going through a military treatment facility, there was a steep discount for the procedure and grants that covered medication costs.
(Majority of insurances offer NO coverage for infertility treatment)
We were looking at $6,300 for IVF and $8,000 for PGS with all meds covered, so the approx. total was around $14,300 at the Naval Hospital.
PGS is short for preimplantation genetic testing. Genetic abnormalities are a frequent cause of early miscarriages in the first third of the pregnancy. Preimplantation diagnosis helps prevent these losses and it provides peace of mind when you are paying such a high cost to have a baby. It is devastating to spend thousands of dollars on a baby that miscarries, especially when it could be greatly avoided through the genetic testing.
With PGS testing you are able to detect the following:
Chromosome defects:
-
- Down syndrome (trisomy 21)
- Edwards’ syndrome (trisomy 18)
- Patau syndrome (trisomy 13)
- Turner syndrome (monosomy X)
- Klinefelter’s syndrome (trisomy XXY)
Gene mutations causing:
-
- cystic fibrosis
- thalassemia
- fragile X syndrome
- sickle cell anemia
- phenylketonuria
- hemophilia
- Alport syndrome
- mutation of tumor suppressor gene p53
- neurofibromatosis type I
Determining the sex of a child whose mother is a carrier of a disease manifested only in boys:
-
- hemophilia A and B
- daltonism
- ectodermal dysplasia
- fragile X syndrome
*By the way, even if you do PGS for peace of mind, you do not have to get the sex results if you are wanting it to be a surprise.
Your clinic/doctor will ask you, prior to providing the PGS results, if you want to know the sexes. If not, they are great about removing them so you can be surprised 🙂
That all being said though, PGS is not required, and since we were trying to save money we were going to decline PGS in order to keep out of pockets costs to a minimum.
Then the doctor dropped a bomb on us that there is a waiting list for IVF and if we get on the list at the end of the appointment we were looking at about 6 months before we could even begin, that would have been around April 2020. This felt like a huge kick to the stomach. (and thank goodness we did not wait as the “spicy flu” of 2020 would have definitely cancelled IVF for us that year)
At this point we have waited, and waited, and waited some more, just to be told there is more waiting to be done. I was over it.
So on our way home I called another clinic that claimed to offer a comparable IVF military price and I booked a consult with them for about two weeks later.
During that time I fought with my insurance to get my referral switched from the military clinic in San Diego to this new private clinic in Oceanside, which was only about 30 mins away from our house.
After a bunch of back and forth, and a few formal complaints filed on my end, I had the holy grail of referrals for my upcoming consult.
At the private clinic I was told that basic IVF was $7,000, PGS was $5,300, and then we would be responsible for the medication as our insurance doesn’t actually pay for infertility meds that are used for IUI/IVF.
I informed my doctor that we didn’t plan on doing the PGS testing as we were trying to save as much money as possible. But he felt strongly that PGS was very important and after talking it over with my husband, we went ahead and included PGS testing.
So all that being said, we decided to proceed forward with IVF at the private clinic because our total costs, including the wonderful PGS testing, was only $12,300. Additionally, there wasn’t a waiting list and we could begin immediately, which was a huge sigh of relief for me.
Our appointment with the private clinic was September 18 and by September 26 we were doing our first round of shots.
We decided to do a “natural conception” month prior to beginning IVF because it turns out, insurance will pay for infertility medication if you are naturally trying to get pregnant on your own. They just won’t pay for it if you are getting help through IUI or IVF..
:eye roll:
Basically the goal here was to order my meds under “natural conception”, and we legitimately did follow the entire protocol for natural conception, this wasn’t an attempt to fraud the system. But when that failed, as we knew it would, we just used the left over meds towards the real deal the following month.
October 26th was Day 1 of IVF for us. I was actually in Kansas visiting family when I was supposed to start my injections, and I am a huge baby about giving myself a shot, so my poor dad was volunteered to stab me in the stomach every day while I was back home.
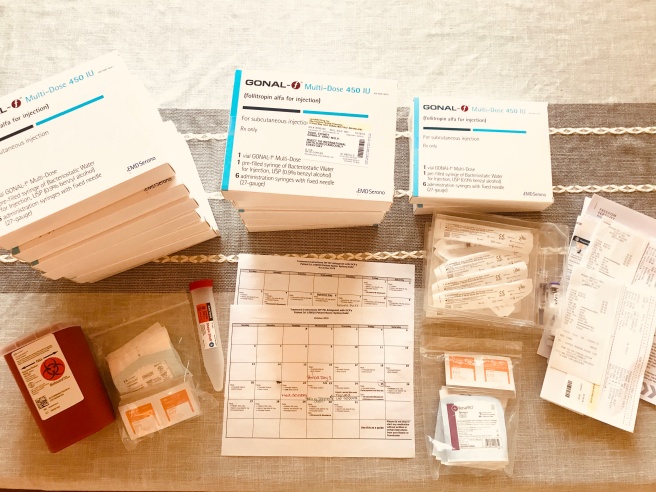

We did 10 days total of injections, called stimulants, or stims for short.
For the first five days I did a single injection every morning of 300 IU of Gonal-F, which stimulated my body to hyper-produce multiple follicles (which is what an egg develops in).
Then the next five days I was doing 2 injections/day.
The Gonal-F and a second injection of Cetrotide, and let me tell ya, IT SUCKED!
The Cetrotide needle was much longer than the Gonal-F, plus the medication would sting really bad and my skin would burn for up to an hour after the injection.
The Cetrotide’s main goal was to block my body from releasing the eggs that had already matured in order to let the smaller ones continue to grow and reach full maturity.

Quick anatomy 101 lesson:
Every month leading up to ovulation, your ovaries develop multiple follicles which your eggs will mature in. Once an egg, or sometimes two, reach maturity your body releases hormones that stops egg production in the other follicles, the mature egg(s) are released which is considered ovulation and when you can get pregnant, and the other eggs that didn’t reach maturity are just flushed by the body.
So the Gonal-F was hyper producing tons and tons of eggs and the Cetrotide was making my body hang on to them by blocking the hormone which would typically trigger ovulation once it detected egg maturity.
These are a few snapshot of the process.
I started getting bruises at my injection sites, so that was fun, and then I spent every 2-3 days at the clinic getting blood drawn and a fancy ultrasound wand shoved up my vag to check on the eggs I was cookin’ up. This is why it’s important you know that we needed a clinic that was closer to us. It would have been a nightmare trying to drive to San Diego every 2/3 days for a 10 min appointment just to check on my levels.
I also took a few time laps videos of Mike being my personal doctor giving me my shots and a time-lapse video mixing meds, because yes, we even had to be chemists for part of this journey.
I’ll be honest, it’s super hard to be short, sweet, and to the point when I am trying to explain IVF stuff. There are so many components that need explained in order to fully understand why other things happened the way they did and so on.
So I again have to quickly pause in order to fill you in about a few key notes from the stimming process.
- Stimming can be very very uncomfortable and I was MISERABLE through the second half of the process. Basically, an organ that isn’t designed to be stretched, my ovaries, is being stretch to its absolute limit. Part of the monitoring they do every 2 to 3 days with the internal ultrasound is to essentially make sure you do not develop OHSS (we’ll talk about this coming up).
I was very very emotional towards the end of this because I was severely swollen and every cough, laugh, hiccup, wrong move, etc. sent shooting pains through my pelvis and abdomen. This was compounded by my injections getting more painful because my stomach was so tender and the second injection felt like injectable fire, on top of having blood draws done every 2-3 days, I was just sick and tired of constantly being uncomfortable in my body and having pain inflicted. - You may be wondering why so many eggs need to be matured and the basic logistics surrounding that event:
The doctor’s goal is to retrieve as many eggs as possibly because the more eggs he/she has to work with the better odds of successfully getting pregnant. A successful retrieval typically is a minimum of 12 mature eggs because at every step in the process you will inevitably lose some. Your doctor wants to have the best odds possible and you need multiple eggs in order to achieve this.
So lets say a women produced 20 mature eggs, theoretically 2 or 3 may not be of good quality, so they’re out, then once they are combined with sperm maybe another 1-10+ do not fertilize/grow, so those are out too, then for the 5-6 days they let them develop into embryos there will be more that stop developing and have to be discarded, then if you do PGS testing you’re going to get some abnormal results, which means you lose more options, and in the end when they transfer your embryo(s) back into your uterus, there is only a 50% chance that embryos is going to stick (we call this moment the “God-factor”).
Some women go through all of this and only end up with 1 or 2 viable embryos and I’ve even seen women where the transfer didn’t stick and they have no other option but to pay another IVF fee and try again or give up. It sucks..
In my case though, I responded really really well to the stimming meds. During my ultrasounds they thought I had somewhere around 36 eggs developing, which is technically good but at the same time was bad because it put me at risk for OHSS, which I told you we were about to talk about ↓ - OHSS is short for ovarian hyperstimulation syndrome. OHSS is an excessive response to taking the medicines (especially injectable gonadotropins) used to make eggs grow. Women with OHSS have a large number of growing follicles along with high estradiol levels. This leads to fluid leaking into the abdomen (belly), which can cause bloating, nausea, and swelling of the abdomen. When OHSS is severe, blood clots, shortness of breath, abdominal pain, dehydration, and vomiting are possible. Rare deaths are reported.
So there ya have it. I was basically straddling the line of mild OHSS towards the end of my stimming cycle. The constant monitoring by the clinic is to watch for OHSS and determine the perfect time for the trigger shot, which I will explain next.
If OHSS gets severe your entire cycle will be cancelled until it goes away and then you can try again with a different treatment option.
In my case, I was definitely uncomfortable from the swelling but it’s terrible to cancel a cycle. So we kept going, monitored it closely, and basically prayed I could make it to my retrieval date. - Last one and then we can move on, the trigger shot is administered when your doctor determines your hormone levels and the ultrasound results have both peaked and the eggs need released. Then your egg retrieval surgery is scheduled within 24 hours of the trigger.
So for me, my trigger shot was approved for the night of Nov. 4th and my retrieval was scheduled first thing in the morning of November 6th.

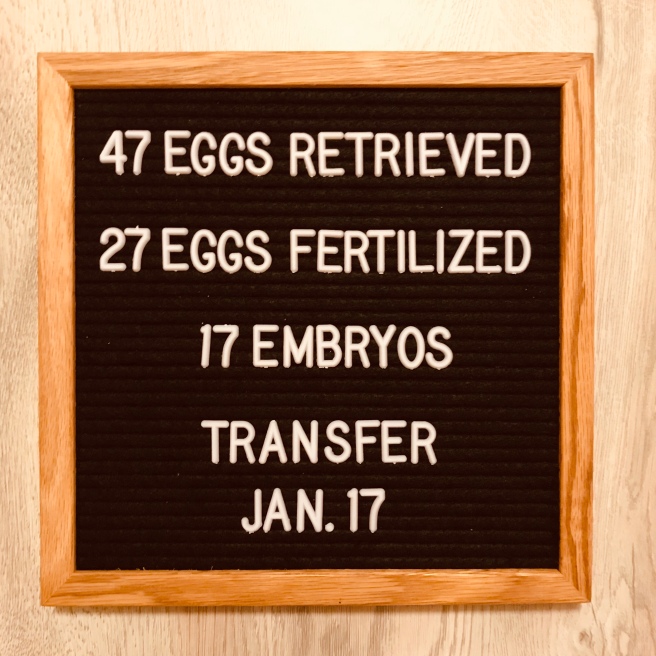
On retrieval day my doctor was able to get 47 eggs!
Guys, that is a sh*t ton of eggs!
He did warn me that my OHSS symptoms may get worse as losing that much fluid so suddenly will make my body respond in shock and it will want to replace it with blood. So my instructions were to basically intake as much salt/electrolytes as I wanted (the theory here is osmosis and having all that sodium will cause the body to pull the blood out of where it shouldn’t be).

The following day we found out how many eggs were successfully fertilized, followed by 5 days later how many were moving on as embryos, as well as our scheduled transfer date.
(the transfer is when they put an embryo back inside the uterus and you hope two weeks later he/she stuck and you are officially pregnant)
Okay guys, I don’t want to stop again and explain the process some more. But unfortunately you need to understand the sequence of events here.
Once the eggs were retrieved they were immediately fertilized with Mike’s sperm, which is the 27 eggs that were successfully fertilized. After 5 days we found out how many made it to embryos, occasionally, there are some fertilized eggs that take their sweet time and do not finish dividing until day 6.
So in our situation we ended up getting 4 more the following day, bringing our grand total to 21 embryos.

Before freezing the embryos, the embryologist carefully biopsies the cells and sent that material off for genetic testing, and then our little embabies are frozen in order to stop the cell division.
In case you are mortified by this process, each embryo is only 70-100 cells at this point. It isn’t a “frozen baby” with developed organs etc., which is a common misconception.
Literally just cells at this point, which is why they can be frozen and thawed, because at this stage they still do not need a “host” to keep them alive. In order to develop organs and real living tissue the embryo has to be attached in the uterus.
It is crucial that they are frozen at this point because in order to survive they now need to be in mama (the host). Well mama’s body isn’t ready for little embaby yet. So that’s why they are frozen until transfer time.
So about 4 days after this we got our PGS results back!
Euploid = normal
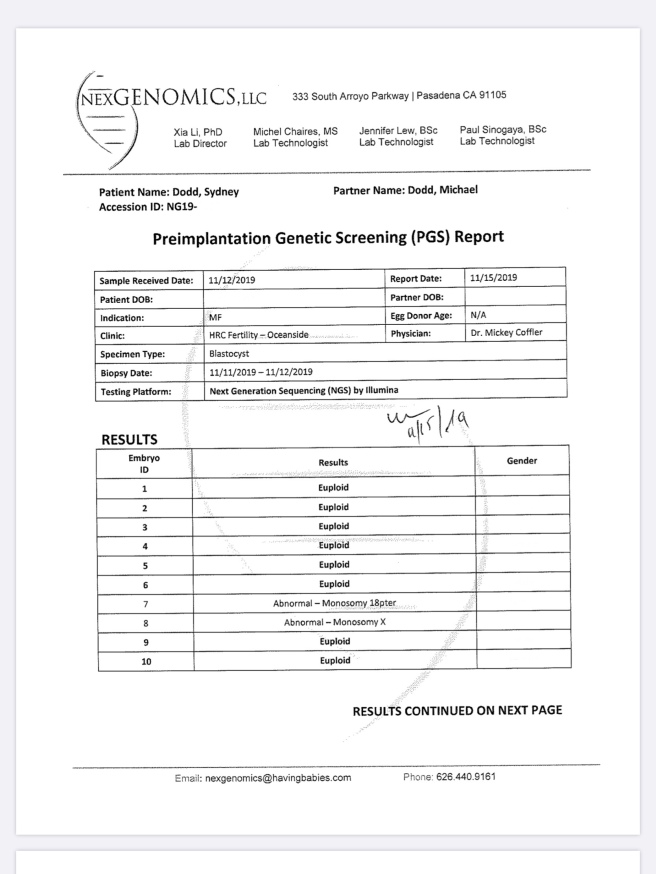
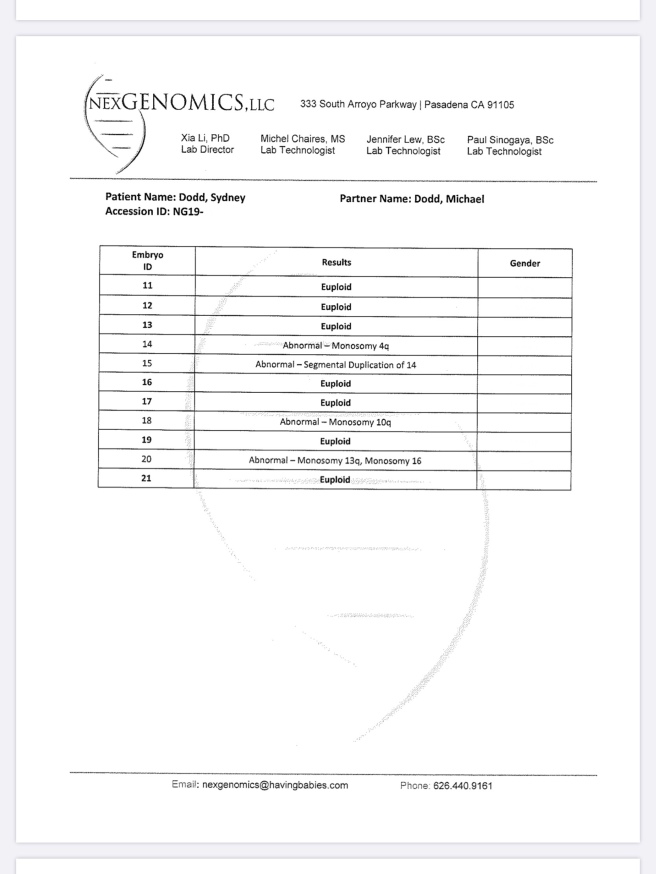
I looked up each abnormal result to see what the monosomy results indicated, call it morbid curiosity if you will. Most of them wouldn’t make it to term, and if they did, the baby would have severe mental retardation and other major deformities.
The most “normal” out of all of the six abnormal embryos was #8 – Monosomy X, which is Turner Syndrome.
During this time my body pretty much went back to normal. The OHSS symptoms went away after about 4 days and my period returned no problem. All we had to do at this point was wait until December 13 when I went in for my next sono/blood work and then I began transfer meds December 16.
We did however have a small hiccup December 4th, which I think was the worst moment during this entire process and honestly I copied over the entire story from my original post because it was drama drama drama and I had no desire to retype and relive any of it.
So forewarning, it’s long.
COPIED FROM MY LONG IVF STORY
“December 6
Last night we received the following email:
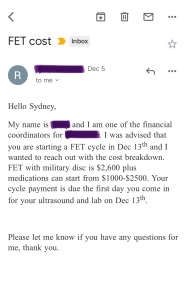
I was completely blind sided as this entire time I assumed putting the embryo back in was included in our IVF costs. I never imagined that we needed to pay an additional $3,600-5,100 after already paying over $12,000…
The transfer has always been discussed casually with my IVF Team and there was never a formal discussion about the cost of an FET (frozen embryo transfer). Additionally, we were never given a choice of fresh vs frozen transfer.
Unfortunately, the fault is on my shoulders. Ultimately I should have asked, I should have been more thorough, and you know what they always say when you assume. It makes an ASS out of U and ME.
IVF is frustrating because none of it is standard and for much of the treatment you need to do your own due diligence and research, which is why there are so many support groups.
In the end, the clinic’s goal is to make money. Sometimes it is hard to differentiate between medical advice that is for my best interest or medical advice that puts more $$ in their pocket. So then you fall back on the advice of other women, but even then, every woman is going through her own IVF process. No one is on the same medication regimen, everyone has different causes of infertility, which is why everyone does different procedures and takes different medication. So navigating your IVF journey is frustrating because what are you supposed to compare it to? It’s not as simple or standard as getting your tonsils taken out..
I am extremely frustrated as I feel we were very misled in the beginning. None of our costs sheets included the FET cost, nor did we have a “treatment plan” that included transfer options.
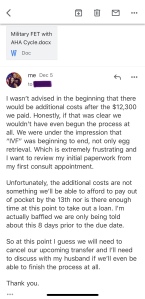
After receiving that email I dug through all of my initial paperwork and went through all of my emails with the clinic looking for something that had FET information or a conversation regarding transfer options. My biggest fear was we unintentionally signed something in the 200 pages of paperwork before we started indicating we would be doing FET.. When I couldn’t find anything I reached out to our coordinator with this email.
But after sending that email I continued to review our paperwork and asked for some advice in my IVF Group. It became very apparent that we are just going to have to swallow this nasty pill if we want to move forward…
What I believe happened is at our first consult, when our doctor sold us on doing the PGS Genetic Testing and I agreed, we were unknowingly and automatically doing a frozen transfer, though this wasn’t ever formally explained or agreed upon. But I have now realized that PGS testing cannot be done for a fresh cycle, it’s impossible. But that shouldn’t have been on me to figure out, I feel that my clinic should have thoroughly explained that process and immediately followed that with the associated cost(s).
If you remember, my doctor had to convince me to even do the PGS testing.
AT THIS TIME is when it should have been made clear that it will also include another $5,100 for the frozen transfer that has to happen if we go that route.
I guarantee if this was clearly explained I would have refused PGS testing, which leads to FET, totaling $10,400, and done the fresh transfer that was included in our initial IVF costs.
•••
Okay guys, I have an update on the above. I scanned over all of my paperwork from our initial consult, as well as my handwritten notes, none of which stated anything about the transfer options or how PGS testing impacts the transfer.
Additionally, I forwarded over 3 different emails where I continually asked for the total cost so we could determine if we were going to take out a loan or if we had enough in savings to cover it. In all 3 emails we were told $12,300 and the cost sheet they attached never included extra transfer fees.
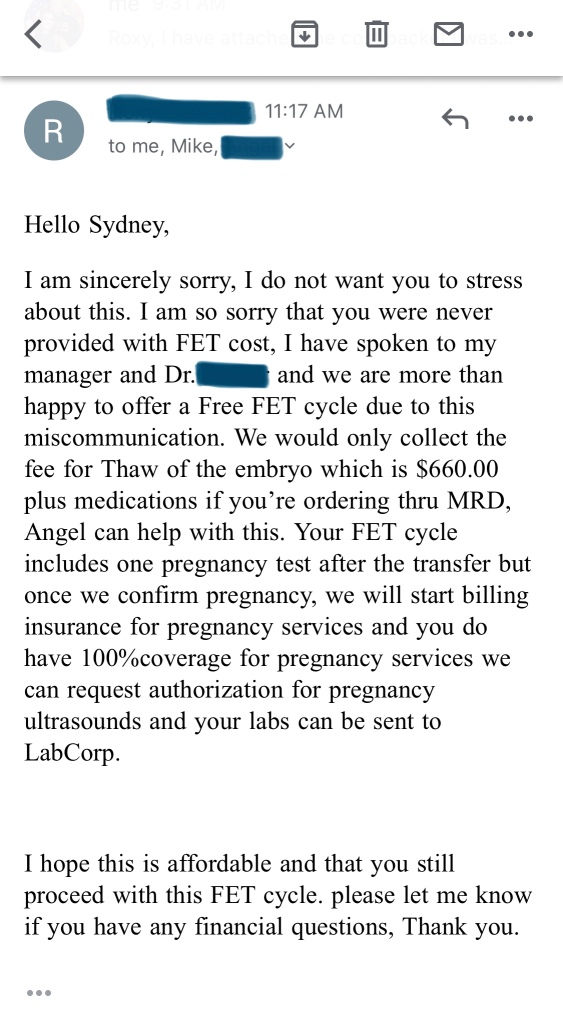
So all of that being said, the clinic informed us they would do the FET for free due to the miscommunication.
I don’t want to beat a dead horse here and keep going over the mishap. So we hit a little hiccup, it was a very stressful 24 hours, but we are moving forward. Lets hope things progress smoothly from here, only 41 days until transfer and so many opportunity for things to go wrong. Let the anxiety begin……”
Mid-December we started transfer meds.
Followed by one last procedure, a hysteroscopy.
A hysteroscopy is the best way to check if your womb is healthy and ready to carry a baby. You wouldn’t bake a cake before checking the oven worked, would you? Same rules apply to IVF cycles. Hysteroscopy is the checker.
First, you’ll be sedated or put under general anaesthesia. Then a narrow tube with a telescope at the end is passed through your vagina and cervix into your uterine cavity, which is sometimes filled with fluid or gas. The images are viewed on a screen and recorded. The surgeon can then check for fibroids, polyps, scar tissue, septa and other malformations. If any are spotted, they can usually be sorted out at the same time – i.e. your hysteroscopy changes from being diagnostic to operative.
Hysteroscopy was smooth sailing! My doctor did find a polyp during the diagnostic portion so he surgically removed it.
From Dec 16 to Jan 16 I just followed my medication protocol and tried to not think about the transfer, just took it day by day.
During this month I slowly increased all of the meds I was on. We even began the most DREADED injection of them all – Progesterone in Oil injections (PIO for short)

They go straight into the fatty area in my hip and they SERIOUSLY HURT. I hate them with a passion. But we gotta stick with it until January 31st until we are in the “clear” and we know Baby Dodd is settled in.

Finally the day all of this preparation was for – Transfer Day!
“January 17
The deed is done! Transfer is complete.
We are officially PUPO – Pregnant Until Proven Otherwise
It was a super easy process and we were legit only there for an hour.

♥
Bottom right pic is our little embaby ↑↑
The next photo is our little embaby officially back where it belongs ♥

We got to watch the whole thing on the ultrasound – Mike even got a video of the embryo going in and being placed.
Now we are home and I am officially on the couch for mandatory bedrest and Mike is making us a yummy breakfast.
I plan on eating tons of “super foods” all weekend and following some old wives tales about consuming pineapple and avocados, laying on my left side, warm beverages and soup (good excuse to have Pho for dinner), keeping my feet warm, staying stress-free, etc.
I will also be catching up on several Netflix series.
Snuggle in Baby Dodd and please stick – lots of people are praying for you ♥”
The last few weeks I have been listening to Tremble by Mosaic MCS on repeat and multiple times a day. The lyrics literally touch my heart every time I listen to them and whenever I am overwhelmed with anxiety and fear over our IVF outcome, I just listen and pour my heart out singing along.
“Peace, bringing it all to peace
The storm surrounding me
Let it break at Your nameStill, call the sea to still
The rage in me to still
Every wave at Your nameJesus, Jesus, You make the darkness tremble
Jesus, Jesus, You silence fear
Jesus, Jesus, You make the darkness tremble
Jesus, JesusBreathe, then call these bones to live
Call these lungs to sing
Once again, I will praise”
Neither of these photos do it justice, the line was so faint I couldn’t get my camera to focus and pick up the line. But in person I could see it (and so could Mike he just wouldn’t admit it)!I could see the hope and I was a ball of emotion. When I first saw that faint positive I felt such relief and excitement, I cried my heart out for a solid 20 mins.
But shortly after that my excitement turned into anxiety – soon after the anxiety came the paranoia.
And sure enough, I watched that little faint line get stronger and darker as the days went on. A week after my first faint positive I did my first blood test which confirmed it:
WE ARE PREGNANT!!!
My team also informed me I will need to stay on all of my hormones and meds until I am considered 11 weeks pregnant, which will be the week of March 15th. (which full disclosure, I stopped around 9 weeks…. I JUST COULDN’T HANDLE ONE MORE PIO SHOT!!)
Next came telling the girls, we initially wanted to wait until middle to end of my first trimester, which would have been March, but the excitement was too real between Mike and I and we had almost slipped and spilled the beans multiple times in that first two weeks.
So our lovely family photographer squeezed us in for this big announcement photo sesh.
The girls just thought we were doing spring family photos and we spent the first 20 minutes taking various family shots all over this awesome location until we finally circled back to the cutest barn where we wanted this surprise to go down.








So there ya have it!
Thats how we got our sweet Baby Dodd. We dreamed and worked for Baby Dodd for 2 years. Lots of prayer, tears, multiple anxiety attacks on my end, lots of medication and surgeries, and in the end lots of laughter and love have all paid off.
We are so excited to welcome this sweet blessing.
The official due date – October 4th, 2020
If you are dealing with infertility – no matter male or female factor – I am always here to listen and talk. I understand the pain and struggle behind seeing other couples welcome babies while just waiting for it to be my turn.
Also, if you have ANY questions about IVF, trying to conceive, etc etc I AM AN OPEN BOOK. During this process, I only had strangers on the internet who tagged their photos with #IVFjourney on Instagram who I could relate to.
Coming out on the other side, I want nothing more than to be a source of information or support for others who find themselves navigating these scary overwhelming waters.And as always, baby dust to you mamas who are praying and longing for it to be your turn ♥
XO
Sydney
































Thank you for all the detail. I am in awe of any couple who have to go down this road. I am sending lots of Angel Love and Blessings. You are an inspiration.
LikeLike